The pilgrimage was a success, emotionally and spiritually, and, for the most part, physically! I even got comfortable with carrying 23 pounds. By the end of the trip, I didn’t even notice the weight, and neither did my arthritic back!
Unfortunately, though, I injured my right knee and didn’t stay off of it enough. The last day of walking pretty much did me in. It was too far—15 miles—too fast on a bad leg. Then I tramped 7 miles across Paris to ascend the Eiffel Tour. Now, I’m back to very low daily mileage, icing and making sure I put my leg up every afternoon. That usually means a nap accompanies the leg elevation, which isn’t such a bad way to spend a rainy fall afternoon.
But most of the other days were rousing successes physically, actually better than I hoped, including the blister prevention and management. Here’s a quick rundown on that aspect of my journey:
Daily rituals—
The morning prepto start walking usually went like this:
- Make sure all strategic body parts (like the sore left ankle) were clean and properly supported with Kinesiotape.
- Kinesiotape the ball of my right foot.
- Tape (usually with Kinesiotape) the second, third and fourth toes to avoid blisters.
- Slather the heals and toes with Foot Glide cream.
- Put the light sock liner on.
- Sprinkle Gold Bond medicated foot powder (to absorb moisture) in the main sock, squish it around for good coverage, and put the sock over the liner.
- Slide gaiters over my ankles before putting shoes on.
- Place lambs wool in the right toe box to cut down on toenail bruising from foot sliding forward in the shoe and banging on the toe box. (This worked wonders! I knew my ballet training with toe shoes knowledge would come in handy some day.)
- Insert foot in shoe and make sure no seams or bunched up sock areas are annoying or noticeable.
- Properly double tie the shoes and attach gaiters to laces and spread them down around the heals and mid-shoe areas.
- Make sure my toes were comfortably spread out while walking rather than scrunched up in the shoes.
Post-walk ritual—
- After peeling off soaked clothes and taking a shower, dry feet thoroughly and check for blisters and hot spots, and then check toe nails, cuticles and rough skin that needs trimming and filing. (I tried to keep my feet and toes as smooth as possible, without grinding off all of the calluses on my big toes and heals. I used a fairly rough mani/pedicure board for this.)
- Walk around the rest of the afternoon and evening in open-toed flip-flops to make sure my feet stay dry. Sometimes my Kinesiotape stayed on in the shower, so I kept it on the body parts it was anchored to the next day.)
- Slather feet with lotion and put socks on to sleep in.
Even with this ritual, which I adhered to religiously, my fourth toes sprung leaks with some nasty blisters; the one on the right toe had two blisters with one under the callus that runs down the middle of my toe. The other toe had a pretty sizeable blister, probably because I didn’t correctly place my blister pressure pad on it a couple of days and ended up increasing the shear rather than decreasing it.

The results—
No matter how hard I tried, I couldn’t keep those fourth toes blister-free, which is probably due to the fact that they curve and twist like little commas, due to all of the time I spent with them hooked around a balance beam while growing up. So I had to do some minor surgery on those.

First steps in dealing with the blisters—
This is where the Spenco 2ndSkin and moleskin strips and cutouts saved my life.
- For several days, I provided extra padding over the blister and around the toe to protect the tender, elevated skin and keep it from breaking. A little piece of Second Skin cut to the length of my toe was placed over the blister and then covered with Kinesiotape or moleskin. If it was just a hot spot I was tending to, I applied a generic blister pad.
- Then I decided I needed to do some lancing of the one blister because it appeared to be getting larger. So I sterilized my cuticle scissors and made tiny slices at the base of the blister and gently pushed the fluid from the blister. Then I went through the same padding procedure.
- But one blister was a toughy. It kept re-sealing itself, so I kept cutting. Several slices on the last go around to make sure it stayed drained. Then I applied the Second Skin and wrapped it across the top and around with moleskin. To alleviate some pressure and attempt to straighten out the toe a bit, I placed a small wedge of lambs wool between the fourth and third toe.
- In spite of pretty fire-red blisters and skin, I walked a lot of mileage without blister pain. Now, about 10 days after completing the walk, I’ve snipped off the dead skin layers. And we’re back in business!
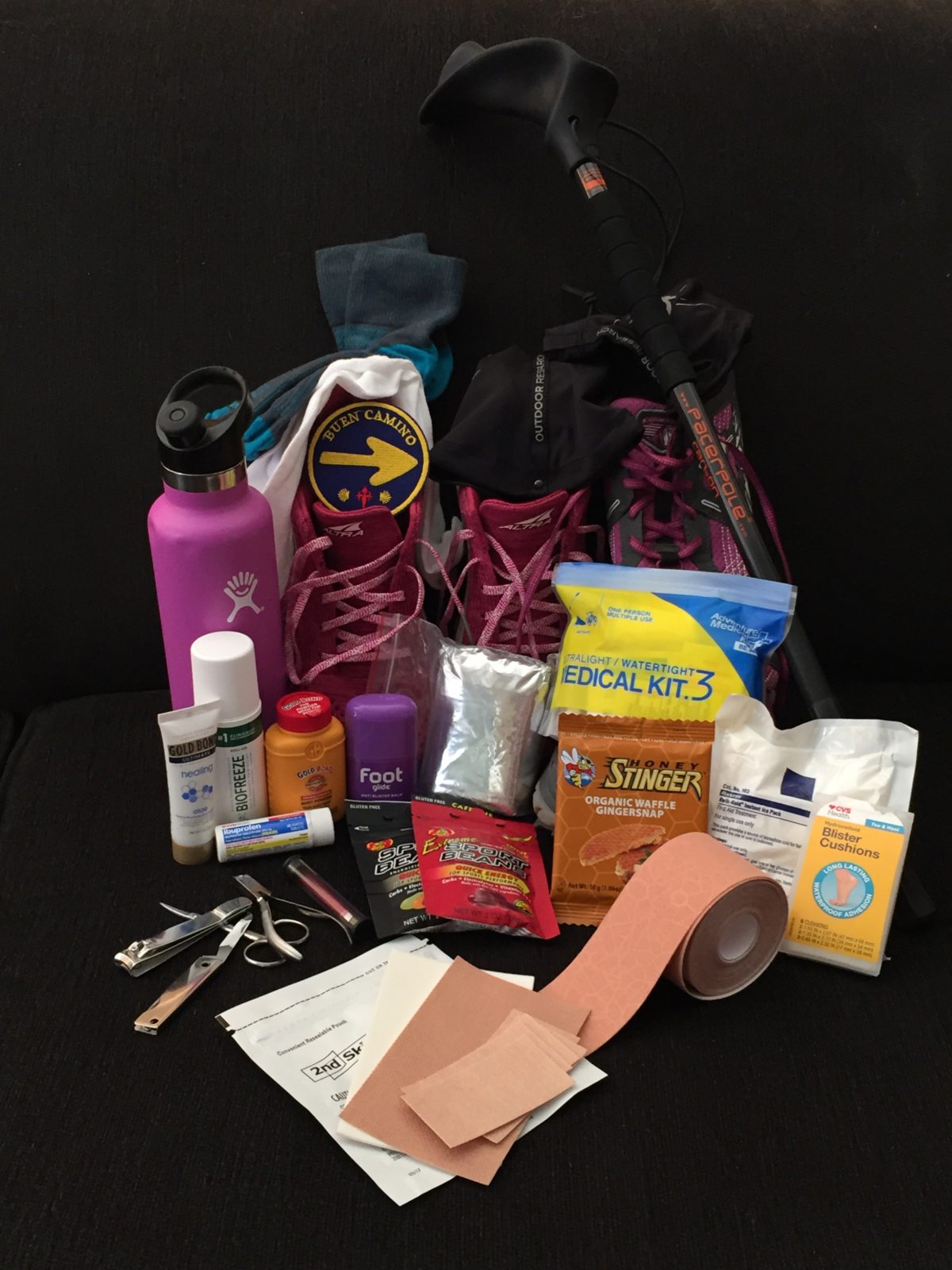
Survival kit—
My toes wouldn’t have survived without my blister care arsenal:
- Foot Glide
- Double-layered socks
- Sock liners
- Drymax socks (these are now my favorite go=to socks!)
- Moleskin
- Spenco 2ndSkin
- Kinesiotape
- Toe clippers and scissors and cuticle clippers
- Told Bond Powder
- Kinesiotape
I also used Desitin Maximum Strength cream for its zinc oxide protection and drying, and its medicated healing capabilities. That was applied at night after a thorough cleaning and drying and before putting on my socks.
Toward the end of the journey, I was measuring and pre-cutting my tape and moleskin to reduce the morning prep time. And I actually had to snap Chris’s Kinesiotape from him to enlist on my feet, legs, knees, and ankles. Good thing for me that he didn’t need it!
Other pilgrims’s foot woes—
We ate dinner one night with a gentleman who was walking the Camino for the second time. He recounted his devastating first experience, with such severe blisters that he couldn’t walk. Some of them broke on their own and ended up getting infected after he showered without wearing shower sandals. Then he contracted something like trench foot. Only after he managed to secure some hefty antibiotic did the infections subside and he finished his walk. It sounded ghastly!
In one of the hostels I watched an older French couple sitting in the lounge. She had her feet on his legs, and he was lovingly applying ointment and bandages to her blistered feet and toes. Her oooh, ooh, ooh’s were replaced by grateful sighs when he carefully slid socks on her feet and tenderly massaged them.
Then, on our last official day of walking, Chris and I encountered a pilgrim perched on a large boulder on the side of the path. Her foot was a mess, and she was trying to improve her predicament by taping a large-wound Telfa pad sheet (like the kind you see with the “plastic” side to control fluid draining and infection) on the bottom of her foot. She had it cut (as closely as possible) to the shape of her foot. I suspect she was trying to reduce friction. It didn’t look as though it was going to turn out so well for her.
She looked miserable.
Not to be taken lightly—
Blister problems can be more than annoying and painful. They can be dangerous. And they need to be taken care of immediately. I’m fortunate to know how to care for blisters and be able to take care of them on my own. But even my blister ailments could have gone south very quickly. The one blister got so red I became concerned about infection. I applied triple antibiotic cream to it for a couple of days as a precaution.
I was fortunate.
Planning and preparing for problems—
If you’re planning any long distance hiking, make sure you prepare your feet well by training, wearing the right shoes for your feet, wearing friction-reducing sock liners and attending to your hot spots as soon as they crop up, NOT after you’ve put in your mileage. If you wait until the walk is over, it might be too late to get control over them. Stay vigilant.
Be prepared.
Make sure you’re all set so you can enjoy the walk!
NEXT WEEK we’ll take a quick look at more equipment you don’t want to hike without. Equipment that can reduce the stress on your joints and feet.
Until then, take care of your feet so they can keep you moving!
Blessings,
Andrea
May you prosper in all things and be in health, just as your soul prospers (3 John 2).
Photo of my own toes taken by me!