AS YOU’RE READING this blog post, I’m either sleeping or out walking on the other side of the world. A dream and Heavenly direction that began a little over a year ago and that has involved months of study, preparation and training has arrived. And my beloved and I are on a life-changing pilgrimage. At least that’s what everyone who has experienced it says it will be, and I have no reason to doubt these friends. That’s the expectation we have.
But preparing for this hasn’t been easy. Especially in the what-to-take category. Most specifically in what to take in case of …
My background in play—
As an athletic trainer, I’m used to carrying around an arsenal of goodies to treat athletic mishaps on the spot. Whether it’s blisters, nosebleeds, dislocated fingers, broken limbs, brain-jarring concussions or spinal injuries, we’re prepared.
While the books I’ve read tell me that the countries I’ll be in really do have nice grocery stores and pharmacies, that won’t do me a lot of good if I have to hobble ten miles through a forest or pastoral farmland before reaching one. So, I aimed to be prepared. But prepared meant a small amount of items in very small sizes. Things that would fit in the portable “house” I’m carrying on my back and help aid my walking comfort and sanity.
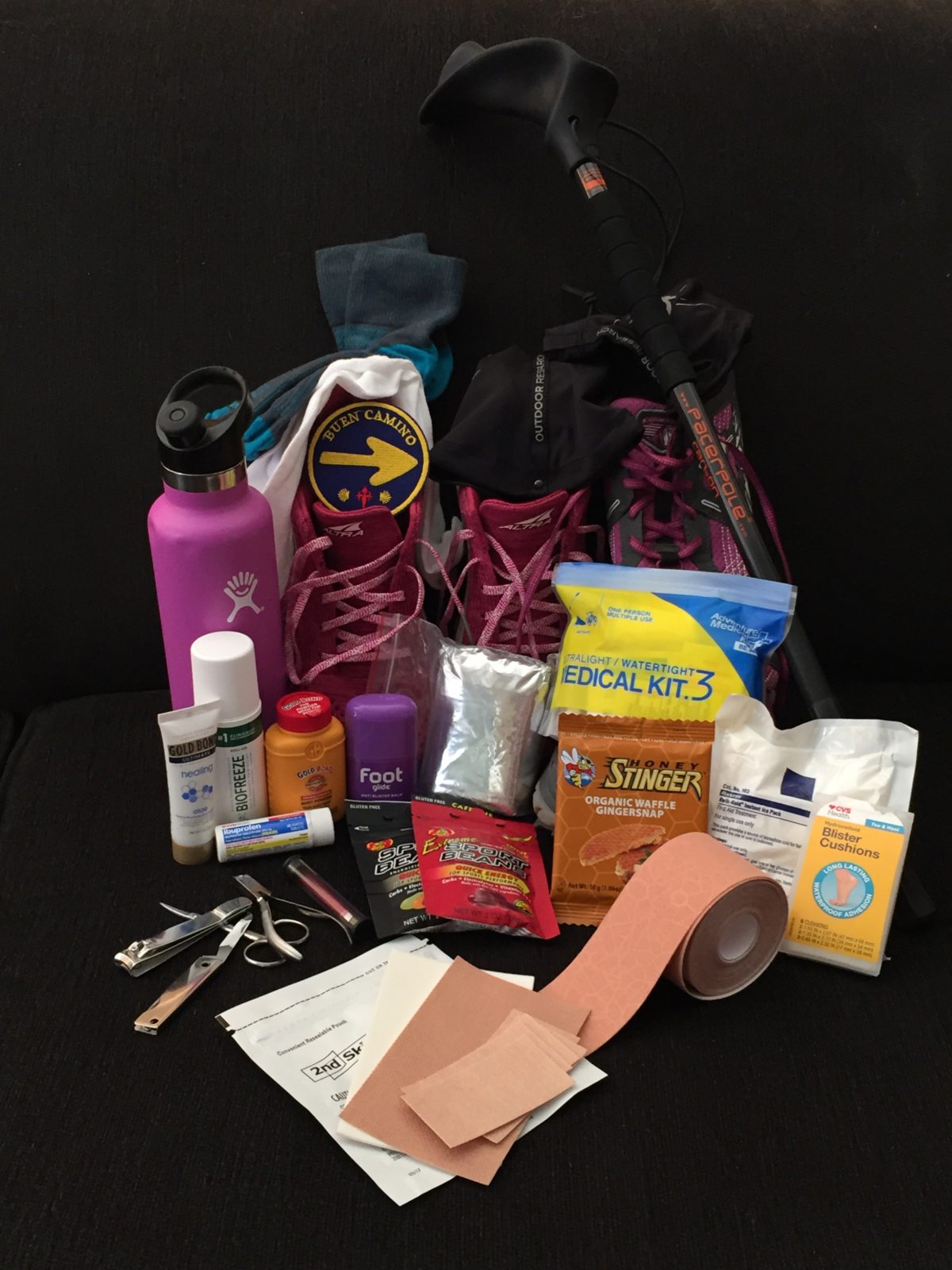
My hiking mini-arsenal for my feet—to prevent and treat foot injuries and blisters—and why I selected these items:
- Two pairs of shoes, a road/trail shoe and a strictly trail pair.
The road/trail shoes provide more support and handle the pounding my feet take on asphalt, which I will be walking on. When I hit the dirt trail, though, I’ll switch to the trail shoes. Better, more lax and forgiving structure for wobbly surfaces.
I had to make the difficult decision to forgo my Keen hiking shoes. I knew I needed to take two pairs of shoes, and the hiking boots are too heavy and too big to fit in my backpack when I’m wearing the other pair. I didn’t want them swinging back and forth on my backpack, either. These Altras are more compressible.
- Hiking Poles!
As I mentioned in my last post, I wouldn’t go anywhere without my beloved hiking poles. I’m taking a pair of poles made in England, called Pacer Poles that my younger son gave me for Christmas. I like them because they help me navigate rocks and take the load off my knees, especially on descents. They’re light and the hand grip has an anatomical/ergonomic slant to it, which helps me avoid irritation to my compressed wrist nerves.
- Water, Water, Water!
As far as my body and I are concerned, one can never carry enough water. I’m prone to dehydration, especially in heat, so I always need to have water available. No waiting until the next fountain makes its appearance. It reduces my chances of suffering a migraine or other effects of insufficient hydration. Even if it adds weight to my pack (and back), I’ll be loaded up.
Staying hydrated also reduces my chances of getting swollen feet.
- Electrolytes
Along with the water, I’ll need to replace electrolytes lost through sweating. I’ve found the Sports Beans brand to help me immensely and perk me up. One bean every fifteen to thirty minutes.
- Energy Snack
I discovered the StroopWaffle-style portable energy snack at Seattle’s REI in June, and I LOVE them. I’ll be taking the Stinger brand with me, because they still make a variety of flavors besides chocolate and caramel, including our favorite ginger flavor. They’re easy to pack and eat on the run (or hike) without too much down time or fanfare.
- Kinesiotape
I’ll be taping my left ankle, several toes, left hamstring, (allowing that to hurt changes my gait and thus overloads my feet), and left outside foot area, and the ball of my right foot. My tape is a godsend to me. It will also be handy in a pinch to cover a hot spot.
- Foot Glide
This is the lubricant I use to apply a light glaze to the ends of my big toes and heals and the ball of my left foot. Works great to reduce hot spots.
- Double-layered socks
These socks are light enough and padded enough to be comfortable in my shoes and reduce the friction and shear forces I’ll confront over miles of walking day after day.
- Sock liners
These will go on under my double-layered socks. They wick sweat away from my foot and provide an extra layer of friction and shear protection. They’re so thin that they don’t provide additional bulk that make my shoes too tight.
- Spenco Second Skin Kit
This will provide me with moleskin and gel pads to patch up any blister that pops up.
- Pedicure appliances
Clippers, nail file, scissors and tweezers are essential to keep my nails properly trimmed and rough and hanging skin under control.
- Gold Bond Powder
I’ll use this to help keep my feet dry and medicated, especially after a shower.
- Lotion
I’m taking a little Gold Bond tube to slather my feet with before bed, but it could be any brand of deep healing lotion. The lotion will keep the calluses down and manageable.
- Ibuprofen
An anti-inflammatory will help in a variety of areas, not just in case of an altitude headache. If my feet get uncomfortably swollen, an anti-inflammatory will help reduce it. It will also help if I suffer a case of hiker’s vasculitis—breakdown of blood vessels under the skin and leakage of blood into the tissues. I hadn’t incurred that problem for years, but it happened one night while hiking just prior to my departure. I have to be careful with anti-inflammatories, though. I was prescribed way too many of them when I was competing, which left my stomach damaged. They can cause internal bleeding and blood thinning, so I tread carefully when using them. Fortunately a little for me goes a long way.
- First Aid Kit
The little kit will provide me with some antiseptic, more ibuprofen, tape and gauze. Little emergency essentials. I can order refills for this bag.
- Emergency reflective blanket
This might not help for my feet, but it will come in handy if one of us gets injured and needs some warmth. Always an essential because you never know what’s going to happen.
- Emergency ice pack
This is the kind you squeeze to activate. It’s a chemical-based, one-type use bag. Good for injuries, swelling and reducing swelling around insect bites. It might come in handy for foot and toe hot spots too.
And, finally,
Gaiters—
These will help keep grit, pebbles and dirt out of my shoes and socks. When worn with my rain pants, they’ll also help keep water out of my shoes. While they’re not specifically made to repel rain, they will slow it down.
That’s a wrap! (No intended.)
That’s my care package. See anything you use or think you’d do well to try out?
I’ll let you know how successful I was at selecting my items when I return!
WORKOUT WEDNESDAYS will be on hiatus until October 19. I’ll give you a foot and blister care wrap-up and then head into eating and diet strategy for brain care and aging. I’ll be sharing some great information I’ll be learning at an October 9 conference.
Until then, choose your first aid kid treatment and prevention kit and supplies carefully to keep your feet in shape to keep trekking!
Blessings,
Andrea
May you prosper in all things and be in health, just as your soul prospers (3 John 2).
Photo by Andrea A Owan